Rowan Foster, one of our ATLAS members, shares her knowledge and experience of comorbid mental health with additional needs and disabilities.
Contents
- Introduction
- Misdiagnosis
- The accessibility of treatment
- Chronic physical illness and mental health
- Lack of services
- Conclusion
Introduction
When someone has additional needs and disabilities, the way they experience the world and consequently the way they experience mental health can be very different, because their brain is wired completely differently – especially in autism. The challenges faced by someone with additional needs and disabilities, living in a world that is not built for them and often works against them, can lead to mental health issues, and in addition to this many mental health conditions are highly comorbid in people with additional needs and disabilities: for example, a study found that seven out of ten people with autism also have a condition like anxiety, depression, or OCD.
In this blog post, I will discuss some of the key issues that young people with comorbid mental health and additional needs and disabilities needs often face.
Misdiagnosis
The way that mental health difficulties can present in young people with additional needs and disabilities needs is highly varied and complex – and as a result, they can be harder to treat. Until you can acknowledge, understand, and meet the needs that a young person with additional needs and disabilities has, it’s tricky to diagnose, understand and treat their mental health difficulties.
Sadly, this isn’t always recognised, and a common result of that is misdiagnosis. Especially when a young person presents with mental health difficulties that need urgent treatment, professionals don’t always have the time or the training to properly take additional needs and disabilities into consideration. But the right diagnosis is crucial to the treatment of any mental health difficulty, because a diagnosis helps a professional decide what treatment needs to be given. Giving the wrong treatment is unproductive at best, and seriously harmful at worst.
For example, some of the misdiagnoses that are given to young people with neurodivergent needs are:
It is important to remember that someone with additional needs and disabilities can still have these mental health difficulties. However, the interaction between a young person’s additional needs and disabilities and their mental health difficulties means that a diagnosis should be made more carefully. To make sure that the right diagnosis is made, there should be professionals involved who are knowledgeable about additional needs and disabilities and how the young person’s additional needs and disabilities affect them must be considered.
A mental health professional I had in the past told me that neurodivergent needs are like a ‘neurological backdrop’ to any mental health problems that show up. It’s like painting on blue vs. red paper. You can put the same paint on the paper, in the same way, but the colour will show up differently.
Professionals can misread the severity of a mental health difficulty because the presentation in a young person with additional needs and disabilities is different to what they expect. With neurodivergent needs in particular, interpreting behaviours and reactions from a purely mental health perspective can lead to misdiagnosis. For example, an autistic meltdown could be misread as a severe mental health crisis, even though it could in fact be relatively easy to manage. If nobody in that young person’s care understands how to do so, they are left untreated.
The accessibility of treatment
Even when a young person is diagnosed correctly, treatments often have different effects on someone with additional needs and disabilities. For example, I have heard repeatedly that many young people with autism struggle with CBT, myself included. This is a therapy that the NHS prescribes for a lot of different mental health difficulties. Nonetheless, the very design of CBT means that it is not suitable for everyone. The best therapeutic approaches are individualised and this is especially true for people with neurodivergent needs.
Many therapeutic settings are not accessible to a young person with additional needs and disabilities, through practical accessibility in some cases and sensory difficulties in others. So even if you manage to get the young person treatment that will work for them, you need to make sure this is treatment they can access. What isn’t always understood about accessibility is that a place isn’t fully accessible if it causes undue stress or difficulty to access it. Even if you cannot see any issues with a young person getting to, from and inside a therapeutic setting, that doesn’t mean they aren’t there.
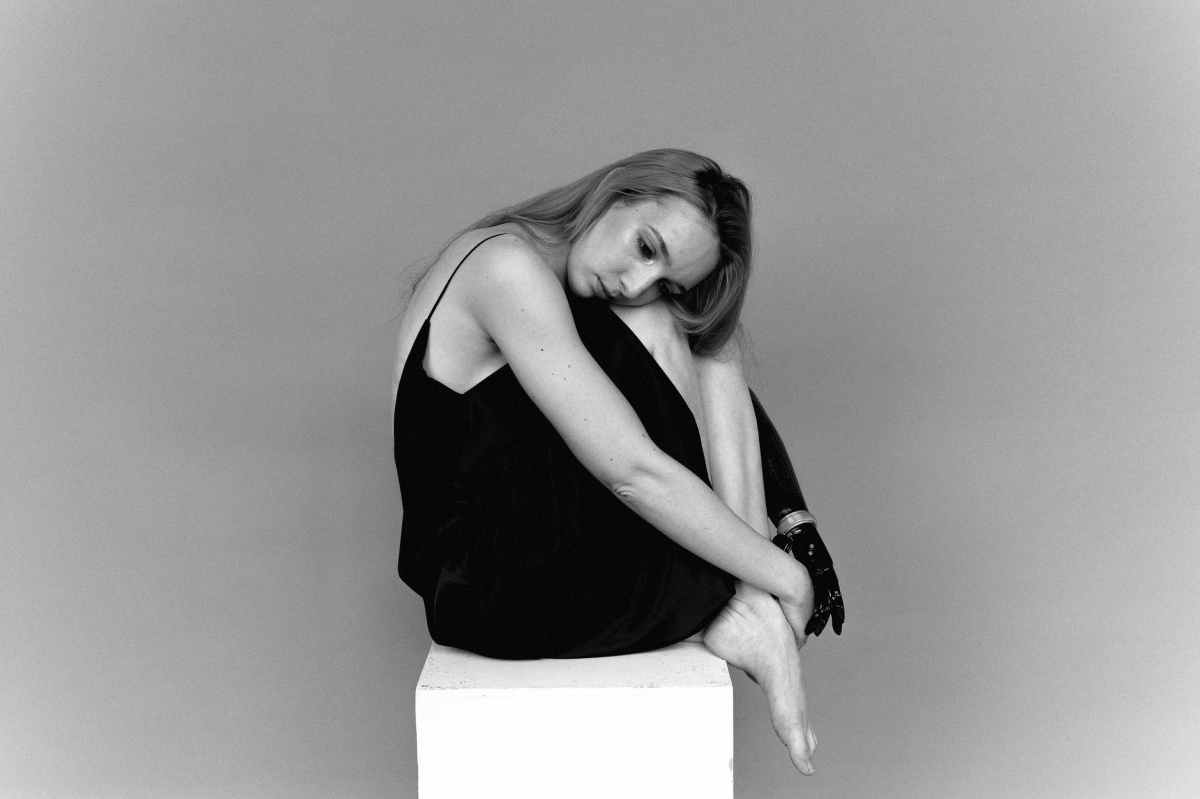
As a person with limited mobility, for example, there are lots of very small things that impact the accessibility of a place – most of which I never would have even thought of when I had full mobility: heavy doors, small steps, the material a path is made from. When the energy and pain it might take for me to get there and back is considered alongside the design of the environment, the recovery time required after an appointment can negatively impact my everyday life.
It is the multitude of small battles that can hurt the most. This is the same for all types of accessibility need. Consider a young person who is anxious about attending a therapeutic setting on top of having to worry about the accessibility of the building they must enter to access support. It is just another stress that they don’t need, and that could exacerbate their existing additional needs and disabilities and/or mental health difficulties.
Imagine that you have been placed somewhere that is supposed to protect you, however it is uncomfortable and possibly painful for you to be there. You are unable to remove yourself from this situation. How do you feel?
Inpatient facilities are often not accessible as they tend to be bright and/or loud spaces with very little privacy: a sensory nightmare. If a young person is there under a section, they cannot leave. Someone in an inpatient facility for their mental health would have been struggling before they arrived. They shouldn’t have to deal with inaccessibility on top of that.
Physical chronic illness/disability and mental health
It is also worth noting that if a young person has physical difficulties like chronic illnesses or disabilities, the relationship between this and comorbid mental health is often not explored in the right way. Young people are often not believed about symptoms like chronic pain – it is assumed that you’re ‘too young’ or exaggerating to get out of doing something. I’ve heard it said before that everything would be better if mental health was treated like physical health, but I’m of the opinion that this isn’t true. Regardless of if your health issues are physical or mental, if someone can’t see it, they often assume it doesn’t exist.
It can be very difficult to access medical treatment or be believed about physical symptoms if you have mental health difficulties, because medical practitioners will often assume that these are the cause. The early symptoms of my physical chronic illnesses were not recognized or addressed by paediatric health services, because they assumed that they were caused by my mental health issues. If they’d been recognized earlier, that could have prevented or at least mitigated the later decline in my physical health.
I have heard of many cases where people are prescribed psychological therapy in the expectation that this will eliminate a lot of their chronic illness symptoms. Therapy can be beneficial for long-term symptom management as it can help you learn to accept and manage your condition however, it is not a cure and shouldn’t be administered as such.
The stress of dealing with physical chronic illness and disability can cause mental health difficulties by itself, especially in cases where pain is involved. It can be so scary for a young person to have to take responsibility for their own body in that way, and it doesn’t help your self esteem when you can’t participate in the same things that your peers do. If your physical illness or disability sets in later in life, then you might also be grieving for the loss of a healthy body.
Young people with physical chronic illnesses and disabilities need empathy and support – and young people need to be believed and listened to.
Lack of services
There is no service or provision for a young person with SEND needs and mental health issues. Unfortunately, this means that nobody knows what to do when a young person needs support for both simultaneously, and nobody knows who is responsible for them. Young people with these more complex needs often find themselves jumping from service to service. The way that the services are built now means that a young person often finds themselves receiving treatment or support from a multitude of teams – none of whom speak to each other. It is usually left up to the young person and their parents or carers to coordinate their own care.
A holistic approach is key to treatment of many mental health conditions, which the current services fail to do. Mental health services do not understand the additional needs and disabilities, and the additional needs and disabilities either don’t have a service (because almost all additional needs and disabilities services are built for young people with moderate to severe visible + physical disabilities or learning difficulties with lower cognitive functioning) or their service doesn’t fully understand the mental health needs, especially when complex. These services can provide some help, but none of them can fully meet that young person’s needs. The fact that they do not talk to each other compounds the issue. The young person is left with a disorganised, often ineffective, treatment path, and it is difficult for them to know what is happening.
Conclusion
I think we need more integrated and holistic care options to provide for the needs of young people with additional needs and disabilities. We face enough discrimination from the world around us. It is disappointing that we sometimes also face this discrimination from the services that are supposed to help us. I believe that we can do better than that. We must.
I hope this post has been a valuable read for you. Maybe you related to parts of it, or maybe you’ve learnt something new. Even more so, I hope that you remember to treat the young people with additional needs and disabilities in your life with compassion and respect. Especially if that person is you.
ATLAS members chose to self-describe with additional needs and disabilities and therefore this article has been updated to replace SEND with additional needs and disabilities.
Resources
[1]https://www.autismresearchtrust.org/news/borderline-personality-disorder-or-autism
[2]https://pro.psychcentral.com/aspergers-syndrome-vs-ocd-how-to-avoid-misdiagnosis/
[3]https://www.drakeinstitute.com/adhd-vs-anxiety-whats-the-difference
[4]https://socialanxietyinstitute.org/social-anxiety-and-aspergers-differences
[5]https://guilfordjournals.com/doi/abs/10.1521/adhd.2005.13.3.9?journalCode=adhd
[6]https://adhdnews.qbtech.com/odd-a-problem-of-misdiagnosis#
[7] https://network.autism.org.uk/good-practice/case-studies/eating-disorder-or-disordered-eating-eating-patterns-autism